Athletic Trainers in the Physician Practice: How they add value and increase revenue
Athletic trainers in the physician practice provide a number of benefits including:
-
Improved performance and productivity
-
Additional revenue streams
-
Higher patient satisfaction
-
Improved quality of life for physicians
This Course Covers
Roles and responsibilities of athletic trainers in the physician practice.
Athletic trainers are valuable to medical practices including sports medicine, orthopedics, primary care, and others because of their specific musculoskeletal training combined with a wide swath of expertise that has the potential to positively impact a physician’s workflow.
Athletic trainers in the physician practice may be involved in:
- Patient triage
- Taking patient vitals
- Taking patient history
- Performing the physical orthopedic exam
- Completing diagnostic exam orders
- Presenting a case to a physician
- Completing surgical or referral/consult forms
- Dictating/scribing the medical record
- Fitting DME and soft goods
- Assisting in the procedure room / operating room
- Patient education
- Concussion testing
- Creating home exercise programs (HEPs)
How athletic trainers in the physician practice impact performance and productivity
Athletic trainers’ impact on performance and productivity can be measured in three main areas.
- RVUs / Charges
- Patient throughput
- Collections
What are RVUs?
Relative value units (RVUs) are measures of productivity used in the Medicare reimbursement formula. They can also be used to compare productivity between providers.
Athletic trainers’ impact on RVUs: For each athletic trainer added to a physician practice, work RVU increased by 3.23 per half-day and 4.3 per full day (Nicolello, et al., 2017).
Athletic trainers’ impact on collections: For each athletic trainer added to a physician practice, patient encounters increased 18% to 22% per day, and collections increased by 10% to 60% per day (Pecha, et al., 2013).
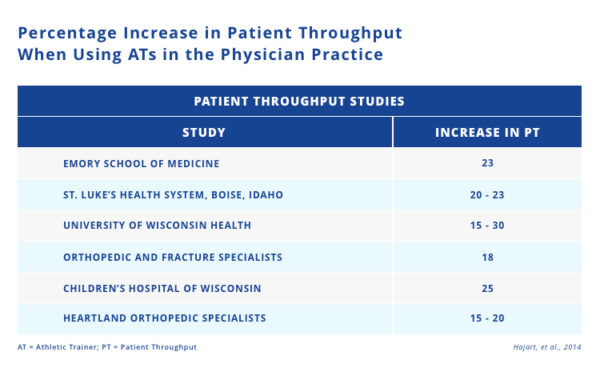
Athletic trainers’ impact on patient throughput: Studies have shown increases in patient throughput between 15%-30% when athletic trainers are utilized properly in the physician practice. On average, there is a 22% improved throughput per athletic trainer per day in a physician practice (Hajart, et al., 2014). We will use this 22% throughput as a benchmark in the calculations throughout this article.
Why is patient throughput important?
Increasing patient throughput has a positive impact on revenue. From the hospital perspective, patient throughput is valuable because assuming that 80-90% of costs are fixed, patient throughput is the determining factor on whether money is made or lost on a particular service. Athletic trainers are able to positively impact throughput by providing services to more patients in the same amount of time.
Patient and physician satisfaction with athletic trainers in the physician practice
Studies have found that patient perception of an athletic trainer in the physician practice is equal to that of an orthopedic resident, despite a difference in the highest level of education attained (Pecha et al., 2015). Additionally, studies have found that patients have a very high level of satisfaction with the technical, interpersonal, and overall care provided by athletic trainers in the physician practice (Acree et al., 2020). This is not surprising since athletic trainers have a lot of technical training and expertise on musculoskeletal conditions as well as experience dealing with sports teams which requires interpersonal skills.
Athletic trainers not only received high levels of satisfaction from patients, but from physicians as well. This study demonstrates the positive impact athletic trainers have on clinical operations as well as physicians’ quality of life. The same study found that when describing the overall skill set of athletic trainers, physicians felt it was very good in comparison to a PA and APN (Nolton et al., 2019).
How athletic trainers contribute to revenue in a physician practice
How much is a patient E/M worth?
Example of the impact of office throughput on E/M revenue:
CPT 99213 - Follow up visit for an established patient (middle level of care)
Medicare rate: $61.73 (2020 Medicare Fee NNJ)
CPT 99203 - New patient visit (middle level of care)
Medicare rate: $132.81 (2020 Medicare Fee NNJ)
Assuming the new vs. established patient ratio is 1 to 4, the expected reimbursement for E/M (Medicare rates) is $79.50.
Using this expected reimbursement amount, if one patient was added a day for a provider who sees patients 3 days a week, this would generate $11,448 in additional annual revenue. Using the same calculation, if 6 new patients were added a day, collections would increase by just short of $80,000 per year.
E/M revenue impact in orthopedic practice: Using the average 22% increase in throughput, the average orthopedic surgeon would get approximately 700 additional visits. With an expected reimbursement of $79.50 per visit, this would generate more than $55,000 in additional revenue from that increase in throughput alone.
E/M revenue impact in primary care practice: Using the 22% increase in throughput, the average primary care physician would get approximately 830 additional visits which would generate almost $66,000 in additional revenue from that increase in throughput alone.
How much is surgery worth?
Emory Sports Medicine did a thorough review looking at their new and returning patient visit value and the percentage of patients that went on to get other services such as physical therapy, surgery, and MRI all to determine what the impact of one patient is on downstream revenue. They determined that their average collections per new patient was $1029.46 (Pecha, Hajart, & Greene, 2012). Emory also reported their revenue per surgery was $1,855. This means that if they were to add one additional surgery a week (assumes 48 working weeks a year) they’d yield an additional $89,040 in revenue a year.
Based on Medicare dollars, revenue per surgery is approximately $1,176.63. Following the same calculation, this would yield $56,478.12 in additional revenue a year with just one additional surgery a week. Using the 22% increase in throughput, the average orthopedic surgeon would get approximately 115 new surgeries which would generate over $134,000 in additional revenue.
How much is concussion testing worth?
According to the Centers for Disease Control and Prevention, there were approximately 2.5 million TBI-related ED visits in the U.S. in 2014, including over 812,000 among children. Many of these concussion patients require follow-up care beyond the emergency room or initial visit. If your practice is prepared to acquire and retain these patients, there’s an opportunity for them to become long-term patients who return for their multidisciplinary care throughout recovery.
The potential for revenue with concussion testing comes from being able to couple reimbursement for concussion testing with reimbursement for the E/M. For this reason, it’s important to use concussion assessment tools that are eligible for reimbursement, and leverage the right billing codes.
Example of the impact of concussion testing on revenue:
CPT 96132 - Neuropsychological testing evaluation by a physician or other qualified healthcare provider
Medicare rate: $58.94 (2020 Medicare Fee NNJ)
CPT 96136 - Neuropsychological test administration and scoring
Medicare rate: $161.86 (2020 Medicare Fee NNJ)
When the two are coupled, there will be a per unit impact of $151.67. Using the previously established 22% increase in throughput, let’s assume patient volume increased from 100 to 122 concussion patients a year, in turn revenue would increase from $15,167 to $18,503.7. This means that adding just one new concussion patient every two weeks can increase revenue by over $3,000.
One often overlooked revenue opportunity for athletic trainers in the physician practice is CPT 99211 which is defined in the 2011 CPT Standard Edition Manual as an office or other outpatient visit that may not require the presence of a physician. There are considerable opportunities to use this code for concussion management, especially if the physician service is minimal or incidental to the overall care provided in the office. If provided under the direction of the physician, you can bill this code assuming the service provided is focused on evaluation and management. For example, if you are assessing and providing care to the patient and administering ImPACT, then using this E/M coupled with the concussion testing code (CPT 96132 or CPT 96136) can pick up the otherwise unreimbursed clinical services provided in that visit.
Northside Hospital (previously Gwinnett Medical’s Concussion Institute) did a 5 year study on the impact that their concussion program had on patient acquisition and revenue and found that it increased their patient volume by 211% and by the fifth year generated almost $500,000 in revenue.
When deciding to incorporate a concussion program in your practice you need to decide if this will be your core business or an ancillary service in your business. If you’re a sports medicine physician, this will likely be a core part of your business as opposed to an orthopedic surgeon who may use it to build relationships with athletic trainers, schools, and athletic programs in the community.
Cost / benefit analysis of employing athletic trainers in the physician practice
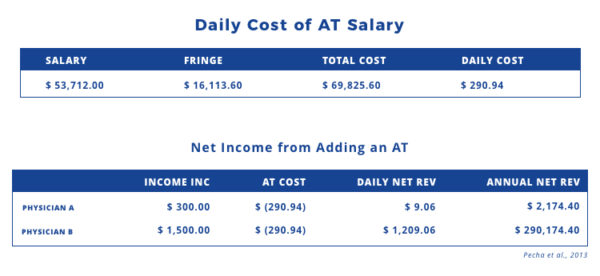
A study on the impact athletic trainers have on revenue in primary care sports medicine and orthopedic practices found that collections increased for physicians with an athletic trainer $300 a day for Physician A and $1,500 for Physician B (Pecha et al., 2013).
The salary estimate for an athletic trainer on average is $53,712 plus about $16,113.60 in fringe benefits. This makes the average annual cost to employ an athletic trainer $69,825.60.
Subtracting this cost from the additional collections generated by employing an athletic trainer, Physician A saw annual net collections of $2,174.40 and Physician B saw annual net collections of $290,174.40 just from having an athletic trainer.
Q&A
Want additional takeaways?
Take the webinar replay course on this topic.
Presented by Aaron Hajart

Aaron F. Hajart, MS, ATC
Chief Operating Officer | SVP Strategy and Innovation
Bergen New Bridge Medical Center
Aaron F. Hajart joined Bergen New Bridge Medical Center in July 2017 and currently serves as the Chief Operating Officer and Senior Vice President for Strategy and Innovation. Mr. Hajart provides executive leadership for hospital operations, strategic planning, managed care, and service excellence.
He joined New Bridge initially leading the transition process for Care Plus Bergen as they took over operations of the medical center as the Chief Transition Officer and served as Chief Strategy Officer prior to his elevation to COO in April of 2018.
*Mr. Hajart is also a contributing author to research on the financial impact of athletic trainers working in the physician practice.